
FREE DELIVERY IN USA OVER $120
We Are Covered by Insurances & Medicare
FREE DELIVERY IN UK / EUROPE OVER $100
Published on: 09/12/2025
Author: John Rainier Yumang
Understanding the correct nurse steps when changing an ostomy bag is essential for ensuring patient safety, preventing skin complications, and promoting long-term confidence in ostomy care. Nurses play a critical role in teaching ostomates how to manage their appliance safely, and their technique forms the foundation of proper at-home routines. This guide follows evidence-based recommendations from leading medical authorities, including the Cleveland Clinic, Mayo Clinic, and the United Ostomy Associations of America (UOAA).
The initial action a nurse takes sets the tone for the entire procedure. Among all nurse steps when changing an ostomy bag, the very first step establishes infection control, patient comfort, and preparation for a smooth appliance change. A rushed or improper start can lead to increased anxiety, improper adhesion, and discomfort.
According to the United Ostomy Associations of America, beginning with a calm and structured approach improves patient outcomes and decreases complications over time.
Here is the complete, evidence-based sequence of nurse steps when changing an ostomy bag, beginning with the crucial first action every clinician should take.
The first and most important of all nurse steps when changing an ostomy bag is proper handwashing. Nurses must wash their hands thoroughly, put on gloves, and ensure all supplies are clean and organized. A sterile environment prevents infection and reduces irritation during the change.
Communication is central to patient-centered care. Nurses should calmly explain what will happen, check comfort levels, and answer questions. This step builds trust and reduces anxiety, especially for new ostomates.
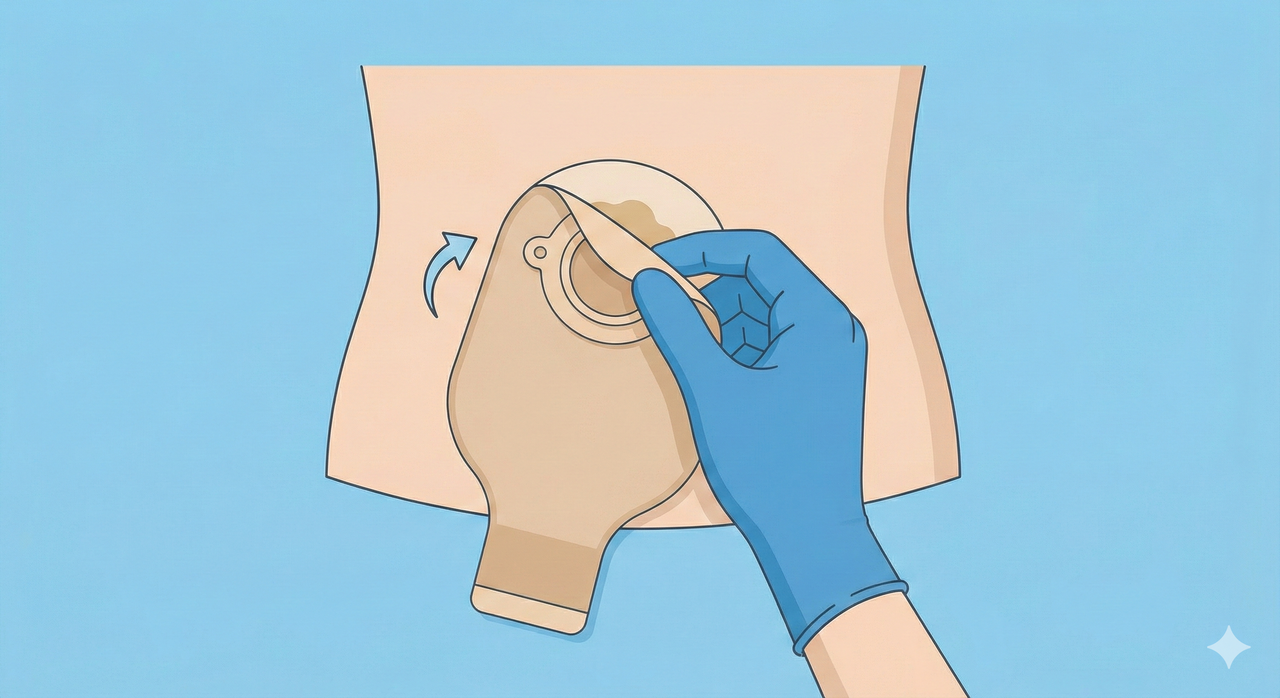
Using adhesive remover wipes or spray, nurses carefully lift the edges of the barrier. This step protects peristomal skin and prevents tearing. Proper technique here forms part of the essential nurse steps when changing an ostomy bag in clinical practice.
The nurse examines the stoma for color, shape, bleeding, and output. They also check for skin irritation, moisture, or signs of fungal infection. Assessment guides any modifications needed during the fitting of the new appliance.
Using warm water and non-woven cloths, nurses clean the area without using soap containing oils or moisturizers. This maintains optimal adhesion and skin health.
Especially important in the months after surgery, measuring ensures the new barrier fits properly. Accurate sizing helps prevent leaks, one of the most common ostomy complications.
Nurses cut the opening (if needed), warm the adhesive with their hands, and apply any barrier rings, paste, or seals. These actions are part of the structured nurse steps when changing an ostomy bag designed to improve appliance wear time.
The nurse centers the opening over the stoma and presses gently to ensure proper adhesion. If needed, support garments like an ostomy belt can be used immediately after application.
Before concluding the change, the nurse teaches the patient how to monitor for issues, how often to change the appliance, and how to maintain skin health. This final step empowers the patient and reduces future complications.
A consistent sequence of nurse steps when changing an ostomy bag stabilizes the patient experience. Structured care prevents leaks, reduces skin irritation, and builds independence. Studies from the Cleveland Clinic demonstrate that meticulous ostomy technique directly correlates with improved comfort and quality of life.
SIIL Ostomy offers products designed to support the success of each step in an ostomy bag change. After applying the new appliance, many nurses recommend stabilizing accessories such as:
These supportive options complement the essential nurse steps when changing an ostomy bag by preserving appliance stability and protecting sensitive skin.
A new patient may feel overwhelmed. When a nurse follows the structured nurse steps when changing an ostomy bag, the patient learns through repetition and consistent guidance.
In cases where output is high, efficient preparation and quick application are vital. Nurses rely on their training to prevent leaks and maintain patient dignity.
When soreness, redness, or fungal infection occurs, nurses adjust the technique and use protective products to restore skin health.
The first step is proper hand hygiene and preparing a clean environment.
Most people change the bag every 3–7 days depending on type and skin condition.
Education ensures long-term success and helps patients manage their care independently.
Yes, especially in the early months post-surgery, as the stoma size may change.
Ostomy belts, stoma protectors, and specialized underwear provide optimal support.
Share this with a friend:
DISCOVER MORE ARTICLES ABOUT OSTOMY
DISCOVER OSTOMY ACCESSORIES:
Written by: Elena Gea, Medical Content Specialist LinkedIn Reviewed by
Most Comfortable Ostomy Supplies for Daily Life Most Comfortable Ostomy
10 Best Ostomy Must Haves for 2025 (Expert Guide) Written
Be the Most informed Ostomate in the world.
Get updated about all the news about Ostomates, new tricks, tips, procedures, ostomy cards, traveling while getting in contact with the biggest ostomy community in the world.


Get Unique Offers and Discounts
Join more than 40.000 Ostomates worldwide in the SIIL Ostomy family and just profit from the offers, information and exclusive discounts just to be member.
Insurances + Medicare +
FSA/HSA
Reimbursement Guide

Download PDF guide👇
SIIL Belts and SIIL Wraps Covered by insurances, Medicare and FSH/HSA.

We hate Spam as much as you do! Your email is safe here.
Score a sneaky
Free Gift!

Don’t sleep on this deal! 👇
We hate Spam as much as you do! Your email is safe here.